The inaugural green light from the Food
and Drug Administration (FDA) for an at-home test targeting chlamydia
and gonorrhea marks a significant stride in the early identification and
treatment of these sexually transmitted
infections (STIs) amid a surging epidemic in the U.S. However, some
advocates for sexual health express concern that the FDA's plan to intensify
regulation of over-the-counter self-testing for STIs might have unintended
consequences.
 |
| Diagnoses of gonorrhea, chlamydia and syphilis have soared in the past two decades |
The pressing need for innovative
tools to combat these infections is evident.
Diagnoses of gonorrhea, chlamydia, and syphilis have witnessed a steep climb over the past two decades. Public health experts argue that this surge is, in part, due to inadequate, long-term, stagnant funding for the Centers for Disease Control and Prevention's (CDC) efforts to curb the spread of STIs.
Anticipation runs high among some
public health officials and advocates that heightened FDA supervision could
legitimize home STI testing, simplifying insurance coverage and potentially
broadening its usage.
While over-the-counter home tests
for these three bacterial STIs are already on the market, the FDA, having never
before sought to enforce regulation or mandate formal approval applications,
cannot guarantee their accuracy.
The FDA's first approval of an at-home test for chlamydia and gonorrhea could help get the skyrocketing STI epidemic under control in the U.S.
— NBC News (@NBCNews) November 26, 2023
But some worry the regulation of self-testing could backfire. https://t.co/x95IpytVmI
A consortium of LGBTQ sexual health
advocates objects to a recent FDA policy proposal. If implemented, this
proposal would necessitate regulatory approval for companies offering at-home
medical tests, including those for STIs. A central concern is that meeting the
FDA's requirements could force some companies out of the STI self-testing
market, potentially escalating the overall cost of tests.
Additionally, there are
reservations about the newly approved test not covering syphilis and
inadequately addressing the needs of gay and bisexual men.
The test kit, known as Simple 2,
does not screen for syphilis, which typically requires at least a finger-prick
blood sample. According to the CDC, there were at least 177,000 syphilis cases
in 2021, marking a 74% increase since 2017. Most worryingly, CDC data reveals a
more than tenfold rise in syphilis rates in newborns over the past decade,
which can be fatal.
Dr. Boghuma Titanji, an
infectious disease specialist at Emory University, highlights that the
inconvenience of having to visit a clinic poses a significant barrier to
getting at-risk individuals tested for STIs.
"Just remove that requirement; that will improve access for many
patients," she said.
Dr. Leandro Mena, director
of the Division of STD Prevention at the CDC, believes that the approval of the
new at-home test will indeed increase testing for gonorrhea and chlamydia.
According to him, self-testing
provides "a tremendous opportunity
to empower people to control when, where, and how they get tested and learn
about their test results, enabling them to get appropriate treatment for these
STIs."
Chlamydia and gonorrhea, diagnosed in 1.6 million and 710,000 people, respectively, in 2021, are the most common STIs in the U.S. They can often be asymptomatic and are easily curable with antibiotics. However, if left untreated, these infections can lead to infertility and can be particularly harmful to women, resulting, for instance, in pelvic inflammatory disease. They disproportionately affect adolescents, young adults, gay and bi men, and people of color.
Will FDA oversight help or hinder
the STI fight?
On Nov. 15, the FDA allowed
promoting approval for grown-ups to involve the over-the-counter Basic 2 Test
for gonorrhea and chlamydia, from the home-testing organization LetsGetChecked.
The test kit, currently priced at $99 through the company's website, can be
activated online, where the consumer completes a health questionnaire before
shipping in samples to a laboratory.
 |
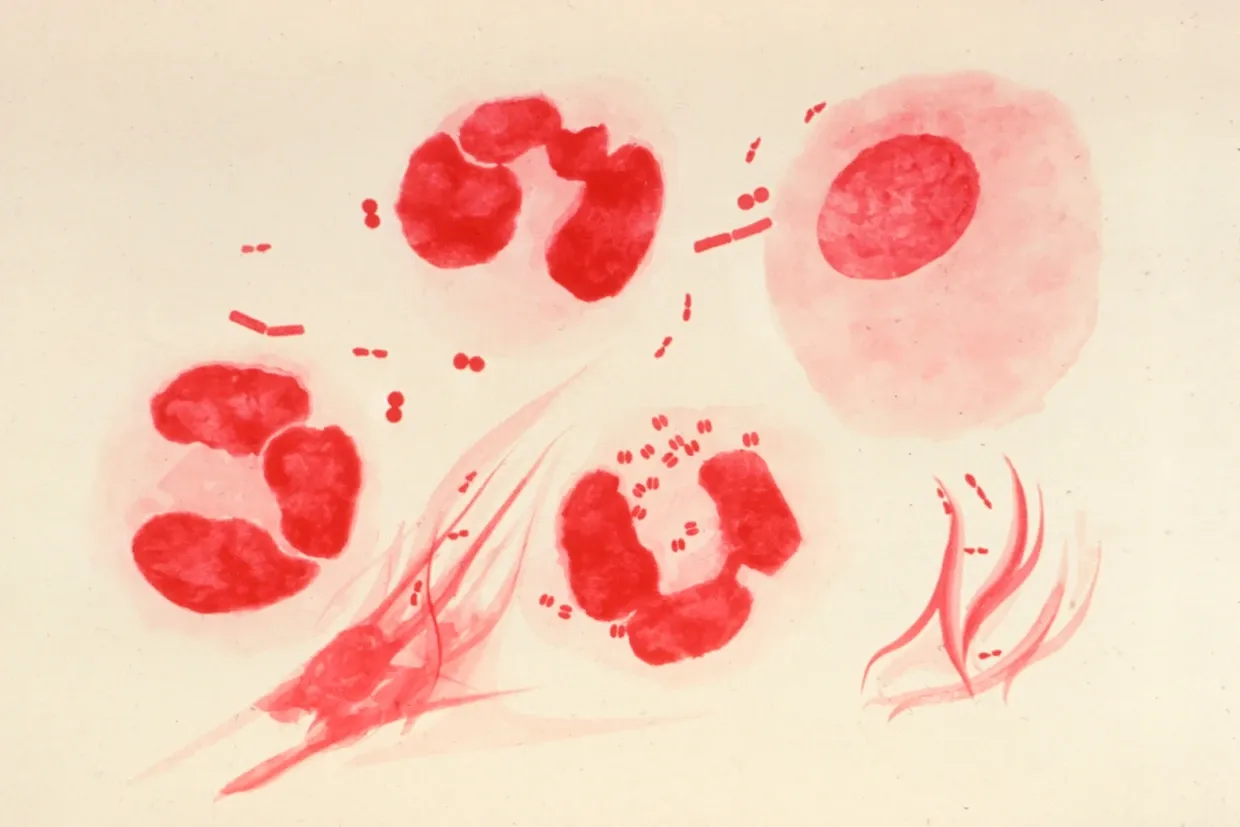
| Neisseria gonorrhoeae bacteria - Neisseria gonorrhoeae causes the sexually transmitted genitourinary infection gonorrhoea |
If the results are positive, the
company would then connect the individual with a physician.
Beforehand, HIV was the main other
physically communicated disease to have a FDA-supported at-home test.
Other at-home STI tests are
available through telemedicine companies and major pharmacy chains. However,
these tests exist in a legal gray zone. Since they're based on samples not
taken in a lab, they don't qualify for an exemption from requiring FDA
approval, a privilege granted to so-called laboratory-developed tests.
The FDA has typically refrained
from asserting control over home-based tests. However, on Sept. 29, the agency
initiated a two-month public comment period on a proposed new plan. This plan
would require companies offering medical self-testing kits for any purpose to
seek formal marketing authorization for their products. The FDA's move followed
reports of defective individual tests that prompted undertreatment or
inappropriate therapy for coronary illness and disease.
The goal, according to the FDA, is
to "ensure the safety and
effectiveness of these tests."
In response, a group including
sexual health advocates and owners of gay dating apps providing free at-home
HIV and STI testing initiated a petition. This petition calls for the FDA to
exempt such public health programs from the proposed new demands. The petition
asserts that gaining approval for existing STI tests would involve a
"time-consuming and expensive process."
Breaking news! @US_FDA grants authorization for a direct to consumer chlamydia and gonorrhea test with at home sample collection! @AlisonFootman @InfoASHA @Beth_Meyerson @kinseyinstitute @SAAFTucson @PPFA @sexualhealthj @CDCSTD @DrMerminCDC https://t.co/OY1lJxHmeX.
— American Sexually Transmitted Diseases Association (@ASTDA1) November 16, 2023
"Many public health leaders are concerned that new FDA regulations will
create additional barriers to public health testing," said Jen
Hecht, director of the consortium Building Healthy Online Communities.
Dr. Matthew Golden, who leads
the HIV and STI control program at Seattle's public health department, notes
that the FDA is playing catch-up in an effort to enforce regulation in an
industry that has grown rapidly since Covid.
"At some level, the horse has left the barn," said Golden,
acknowledging that self-testing kits have been widely used for years. However,
he remarked that for "some of those
tests, how well they perform is not well known. So cleaning this up makes
sense."
A source familiar with FDA policies
and practices informed NBC News that if the agency decides to demand that
self-testing companies obtain regulatory approval, it would not likely
interrupt the availability of existing medical self-tests during the
application process.
However, once a critical mass of self-testing companies obtained or otherwise sought approval, the agency would likely pursue any laggards.
Gay men's needs are left out — for
now:
The Simple 2 Test is effectively
tailored only for STI exposures from vaginal intercourse.
The unit can handle a pee test and
a swab of the vaginal region. Chlamydia and gonorrhea contaminations, in any
case, can be confined in the throat, urogenital region, or rectum. A pee test
can identify urogenital diseases in people. For the individuals who might have
been uncovered through oral or butt-centric sex, oral and rectal swabs would
likewise be vital.
 |
| A urine sample collection tube for chlamydia PCR |
David Harvey, executive
director of the National Coalition of STD Directors, states that public health
experts "anticipate and require"
the FDA ultimately to approve at-home tests for syphilis and for oral and
rectal gonorrhea and chlamydia infections, "so we're also reaching others who are at high risk, including gay men."
The CDC's Mena expresses hope that
the agency and the FDA will consult with LetsGetChecked or other testing
companies about pushing for additional approvals.
The FDA's authorization for the
Simple 2 Test was based on data indicating that consumers could successfully
use the home tests, comprehend the results, and then take any necessary
subsequent action.
It remains uncertain whether the
test will be available outside the LetsGetChecked website or whether the $99
kit will be covered by insurance. The company didn't respond to requests for
comment.
Tristan Schukraft, CEO of
MISTR, a telehealth company providing the PrEP HIV prevention pill, supports
increased FDA oversight of home tests but expresses concern that tighter
regulation could inflate the cost of testing.
"Labs will be required to allocate additional resources to studies,
quality systems, reagents, and software systems," Schukraft said.
Additionally, MISTR mandates that
PrEP recipients undergo testing every three months for chlamydia, gonorrhea,
and syphilis. At least 85% of MISTR customers on PrEP choose at-home testing.
The company advises those who test positive — about 13.5% of the kits detect at
least one STI — to seek medical care and offers assistance in connecting
individuals to care as needed.
Schukraft suggests that greater
regulation could prompt companies to withdraw such tests from the market.
If so, he asserts, "the FDA would be doing harm to public health."
Frequently Asked Questions (FAQs):
What is the significance of the
FDA's approval of an at-home test for chlamydia and gonorrhea?
The FDA's approval of an at-home
test for chlamydia and gonorrhea is crucial as it could facilitate earlier
detection and treatment of these sexually transmitted infections, especially
amid a rising epidemic in the U.S.
Why are there concerns about the
FDA's proposal to increase regulation of over-the-counter self-testing for
STIs?
Some sexual health advocates worry
that the FDA's proposal to intensify regulation of over-the-counter
self-testing for STIs could have unintended consequences. There are concerns
that it might drive some companies out of the STI self-testing market and
potentially increase the overall cost of tests.
What is the current state of STIs
in the U.S. according to public health experts?
Diagnoses of gonorrhea, chlamydia,
and syphilis have surged in the past two decades. Public health experts
attribute this increase, at least partially, to long-term flat funding of the
Centers for Disease Control and Prevention's budget dedicated to combating the
spread of STIs.
How do the LGBTQ sexual health
advocates respond to the FDA's policy proposal?
A consortium of LGBTQ sexual health advocates objects to the FDA's policy proposal, expressing concerns that meeting the FDA's demands could lead to some companies exiting the STI self-testing market and potentially driving up the cost of tests.
Why is there a concern about the
newly approved test not covering syphilis?
The newly approved test, called
Simple 2, does not screen for syphilis, which typically requires a finger-prick
blood sample. This omission is concerning, especially given the significant
increase in syphilis cases in recent years.
How does the Simple 2 Test work,
and what does it cover?
The Simple 2 Test, granted FDA
approval, is designed for gonorrhea and chlamydia testing. It involves a
process where consumers activate the test online, fill out a health
questionnaire, and then ship samples to a laboratory for analysis.
What is the stance of public health
officials on the FDA's plan for increased regulation?
While some public health officials
expect that greater FDA oversight will legitimize home STI testing, making it
easier to obtain insurance coverage and expanding its use, there are concerns
that the proposed regulations could create barriers and drive up costs.
Are there existing at-home STI
tests, and how are they regulated?
Yes, other at-home STI tests are
available through telemedicine companies and major pharmacy chains. However,
these tests exist in a legal gray zone, as they are not taken in a lab, making
them ineligible for FDA approval exemptions.
What are the potential implications
of increased FDA oversight on home tests, according to advocates?
Advocates express concern that
increased FDA oversight could potentially lead to additional barriers for
public health testing, as companies may face higher expenses and regulatory
hurdles, affecting the accessibility of at-home tests.
How does the article address the
needs of gay and bisexual men in the context of STI testing?
The article highlights concerns
that the newly approved test, Simple 2, is not well-suited to address the needs
of gay and bisexual men. There are calls for approvals for tests covering
syphilis and oral and rectal gonorrhea and chlamydia infections to address
high-risk populations.

0 Comments