Florida is currently facing a
measles outbreak, with nine mainly children infected. Despite this, Florida
Surgeon General Dr. Joseph Ladapo went against Centers for Disease Control
guidance and told parents of unvaccinated children they can decide whether to
keep their children home from school during the outbreak. The current
recommendations state that unvaccinated children should stay home for 21 days
after exposure.
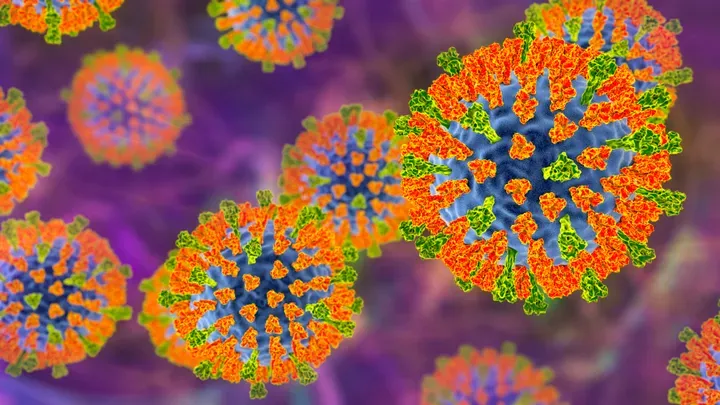 |
| KATERYNA KON/SCIENCE PHOTO LIBRARY VIA GETTY IMAGES |
Experts emphasize that measles is a serious disease, particularly for those who aren’t protected. "What most people forget ― because we haven’t had a lot of measles in the United States for a long time ― is that measles can be a relatively serious disease," said Dr. Mark Roberts, a distinguished professor of health policy and management and director of the Public Health Dynamics Lab at the University of Pittsburgh School of Public Health.
Measles begins with respiratory
symptoms like coughing and sneezing and progresses to inflamed eyes, high
fever, mouth sores, rash, and more severe issues, said Dr. Gary Reschak, a
pediatrician at Northwestern Medicine Huntley Hospital in Illinois.
"Between 130,000 to 140,000 children die annually from measles in
regions with low vaccination rates and limited access to vaccines,"
stated Roberts. According to the CDC, approximately 1 to 3 in 1,000 measles
cases lead to death. Roberts emphasized that measles is more than just a rash.
Reschak explained, "When you contract measles, it weakens your
immune system, making you susceptible to secondary infections. Many severe
complications of measles result from these secondary infections."
Common secondary infections in
children include pneumonia, diarrhea, and ear infections, Reschak noted.
Encephalitis, or brain swelling, occurs in an estimated 1 in 1,000 cases of
measles, leading to lifelong neurological damage.
The situation is concerning, but fortunately, there is a highly effective vaccine available. However, the challenge lies in the declining rates of vaccination among children. What does this mean for us? Experts elaborate below:
More outbreaks will occur if
measles vaccination rates continue to drop
As of the 2021-2022 school year,
roughly 93% of kindergarten students had received their measles vaccine,
according to the CDC, with the target percentage being 95%. However, we're
seeing more outbreaks, such as the current one in Florida, in populations with
high rates of unimmunized children across the country, Reschak said.
Roberts added that so far, the
United States has been fortunate in that the outbreaks have been relatively
small. There were relatively small occurrences in Disneyland, California, in
2014, and one in Ohio in 2022. However, if just one infected child comes in
contact with a community with low vaccination rates, an additional 15 to 16
kids can be easily infected.
"So, it can explode relatively quickly if you happen to get people who are not vaccinated," Roberts explains.
Measles is highly contagious,
spreading quickly through direct contact with an infected person, as well as
through sneezing, coughing, and touching contaminated surfaces like desks or
doorknobs, both experts said. Reschak emphasized that measles is in a league of
its own in terms of contagiousness, unlike the cold, flu, or even COVID-19.
"Measles is not something you can
wash your hands to avoid," he explained.
Moreover, measles can linger in a
space long after an infected person has left. For instance, if you're
susceptible to measles, meaning you lack immunity or haven't been vaccinated,
you could enter a room where an infected person was two hours prior and have a
90% chance of getting infected, Reschak noted.
Roberts added that the higher the infectiousness of a disease, the higher the percentage of immune individuals needed to achieve herd immunity — the level of immunity in a population necessary to halt the spread of an infectious disease.
“Measles is just about the most infectious disease that’s around ... and
you need about somewhere in the middle 90% of people to be immune before you
get herd immunity with measles,” Roberts said.
Once the vaccination rate drops
below 90% in a school, for example, it can lead to large outbreaks stemming
from a single case.
Roberts, who helps facilitate the University of Pittsburgh’s online measles simulator, which models the spread of measles in various communities in the United States, explained, "When we modeled the actual vaccination rates and what would happen... there were schools in Texas where only 40% of the children were vaccinated. If you introduce a case of active measles into a school with only 40% vaccination, it can lead to hundreds of cases."
The vaccine won’t be 100%
protective for everyone. So if herd immunity isn’t achieved, more people are at
risk
The most vulnerable to measles are
those who are unvaccinated. The majority of vaccinated individuals are
protected, but in some cases, vaccinated individuals may not be fully
protected, Reschak explained.
The current measles vaccine
schedule includes two shots, one at age 1 and a booster at age 5. "The majority of adults reading this likely
went through a similar vaccination process," Reschak noted. After one
dose of the measles vaccine, there's a 93% chance of immunity. However, there's
a 7% chance that the vaccine isn't fully effective, which is a normal aspect of
vaccination.
With two doses, the immunity rate increases to 97%, leaving a 3% chance of susceptibility to measles. While this is a low number, it still accounts for individuals unsure of their vaccine's effectiveness.
Furthermore, certain children, such
as those with cancer or immune diseases, may be unable to receive the vaccine.
Some children may also not produce an immune response to the vaccine, similar
to adults. "The highest risk groups
for measles are children under 5, adults over 20, and those with compromised
immune systems," Reschak emphasized.
Groups such as babies too young for
their first measles vaccine or adults undergoing chemotherapy face higher risks
from measles, Reschak noted. Pregnant individuals are also at a higher risk of
complications from a measles infection, according to the CDC.
"Herd immunity is crucial here. When only 3% of the population is
susceptible and everyone is vaccinated, the spread of measles is limited.
Measles can't easily spread," Reschak explained. "But as vaccine rates drop, there are enough
unvaccinated people for measles to circulate."
The most effective way to protect oneself and others from measles is vaccination, Reschak emphasized. While the vaccine provides high protection, there's still a 3% chance of susceptibility even after vaccination. If you're unsure about your immunity status, you can consult your doctor for testing, but Reschak noted that this is typically unnecessary for most people.
Continuing to let unvaccinated kids
go to school will increase risk
Roberts emphasized that the decision to allow unvaccinated individuals to attend school not only jeopardizes those individuals but also endangers those who cannot be vaccinated or are not fully protected. He believes this is primarily a public health issue rather than a personal decision, asserting that as public health experts, there is a responsibility to safeguard the entire population.
In conclusion, the measles vaccine
is safe and plays a crucial role in public health. Despite misinformation,
Roberts stressed that the vaccine is safe and has been administered to hundreds
of millions of people, providing lifelong protection from measles.
Reschak advised seeking information
from healthcare providers rather than relying on internet or social media
sources. He urged individuals to consult with their provider or pediatrician
for accurate information to ensure the safety of their children and family.

0 Comments